Baby Alarico's Birth Story
Short story:-
Alarico was born by emergency c-section on Friday the 28th of June 2013 at 16:25 MT. He was 7lbs and 19.5 inches tall. We are both healthy and happy!
Long story
At our 40 week appointment, I was 1cm dilated, 50% effaced and the baby was at -1 station. I had a membrane sweep to move things along. I started to lose my mucous plug shortly after. On Tuesday I had my first painful contraction, breathed through it and thought, 'Yay! This is really going to happen!' We'd planned for an all natural birth with an out of network birth centre and I was so excited that labor was starting because they are not allowed to deliver babies when the mother is past 42 weeks gestation. By 3am Wednesday morning, the contractions started to be timeable, and I was having them regularly around 15 minutes apart. They then started getting closer together, to where I was ranging between 3 and 15 minutes apart...for the next two and a half days. These were not Braxton Hicks, these were the kind of contractions that stopped me in my tracks and had me holding onto furniture and moaning in pain. Our birth centre will only admit you when you've had contractions at 3 mins apart lasting a minute for at least an hour. At one point it was close, and I was exhausted. We called the on call midwife, who told me to take a hot bath, drink some gatorade to get some energy back and try to get 4 hours of uninterrupted sleep. I tried it, and I was able to get about two hours of sleep with only a couple of mild contractions in between. When we called back the midwife she said that the fact that the bath didn't speed up labor meant that this was still early labor and that I should wait it out until '3-1-1'.
By Friday morning, V and I were both completely exhausted. She'd been timing all of my contractions since Tuesday, to the point where her contraction timer app had maxed out, and we had bits of paper all over the house with contraction times written down. At this point I was starting to doubt that I was strong enough to even go through with a natural birth. I've always thought that I have a high pain threshold, but if this was the pain of early labor, I couldn?t imagine getting to the end. I explained to the midwife that I had a sharp pain low in my pelvis every time I contracted, and she asked if I was a first time mum and then explained that that was normal for my stage of labor. I even contacted my primary care OB nurse for a second opinion. She was sweet, but came to the same conclusion as the midwife. This renewed my waning confidence in the model of care, but still scared the crap out of me. I really wasn't sure that I could handle much more of the pain, and of course after laboring for almost three days I was a little delirious.
Friday at Noon, we had a scheduled 41 week appointment at the birth centre. The midwife did an ultrasound to check fluid levels. They wanted to see at least 5 (cm, I think?) we measured at 8. The midwife did say that there was one quadrant of the uterus that she couldn't count because it had too much cord in it. His heart seemed fine too. Otherwise, she said things checked out for that test. Next was an internal exam. I had my heart set on being at least 3cm dilated. I was so tired that I thought this kind of progress would give me a bit of an emotional boost to keep going. The student midwife who did the internal check had been an OB nurse for 6 years, and looked really confused when she did the check. She said that she hadn't asked for anyone to do a second check of her exams before, but that she thought I was 6cm dilated and they didn't expect that at this point, so she was really surprised. The midwife did another check and said that I was definitely a 'stretchy' 5cm dilated. At this point I was so excited. I'd been having contractions so painful that I'd been in tears while I was having the exam, so being this dilated made me feel like at least I was making progress. The trainee midwife had felt my belly while I was contracting and said that she could tell these were really strong contractions. The next part of the test was to go upstairs for a non-stress test which involves being strapped into some monitors which monitor both the baby's heart beat and my contractions simultaneously for about 20 minutes. After a while of V and I being really excited about my progress, we decided to take a look at the graph that the monitor was spitting out. We noticed that his heart beat was dropping to 105 beats per minute when I was having a contraction. I knew that this was a bad sign. The student midwife came in to check on the list, and quickly said that she'd take it for the midwife to look at. I started to get a little bit nervous. The midwife came in and said that because she was seeing some dips in the heart rate, they were calling in the on call midwife for us and would have her monitor the results more closely for another 20 minutes or so. She then turned me on my left side for a while. This made the decelerations worse, so we moved me to my right side. The on call midwife arrived in about 10 minutes. As soon as she came in, she said hello, stroked my hair and held my hand through a contraction, and then went straight to the printout and told us that she was sorry but that we would not be able to give birth at the birth centre and would need to transfer to the hospital. She said that they don't like to see the heart rate go below 120 bpm and that we'd dropped well below that several times. I am with Kaiser, and asked her which of the local Kaiser hospitals was better to transfer to, since this wasn?t an emergency. She said that we didn't have time to drive to either, and she'd like us to go to the non-Kaiser hospital directly across the road for continuous monitoring. This is where I started to panic, and was in tears again. Veronica called her mom and let her know we were transferring.The midwife made a couple of calls, one to the hospital to let them know that we were coming, and one to have an on-call doula meet us at the hospital. We then quickly got into the car and V drove us and the midwife over to the hospital. V?s mum made it just minutes after we did.
The midwife walked us up to Labor & Delivery, helping me through a couple of contractions on the way. Once in L&D I was given a gown and put straight on monitors again. One nurse implied that the midwife was being a bit dramatic, and played down the heart decelerations, as normal dips in heart rate called ?variations?. I had a few more contractions while the nurse took my information and had me sign some consent forms. The nurse had me lie on my left side, despite the midwife telling her that that was the side where we'd had the worst dips in heart rate. This is where things started to feel like an episode of Gray's Anatomy for me. All of a sudden a doctor came running into the room and shouted, 'Turn her over now!' V told me later that at this point his heart rate had dropped to 86 and was very slow in coming back up. I could hear the slowing of the monitor, which terrified me. V had asked them to turn down the volume to keep me from panicking, the midwife did briefly, but then someone turned it up again. I moved onto my right side and looked up and there were about 10 people in the room. Someone gave V an epidural consent form to read to me and get me to sign, and someone else asked if they could do an internal exam. V asked if she should wait until after the exam to read the form to me, and they replied, 'No, get it done as soon as possible.' The first internal exam again confused the person doing it, so she asked the obstetric surgeon to try. (By the way, this person had hands like the hulk and should never have been in OB medicine!) The surgeon (with little petite surgeon hands - thank goodness) did a second exam and said that the baby was presenting face first, and this is what was stalling our labor and making it so painful. She also tried to move him at this point, but she couldn?t. Because we'd been in labor so long, the baby was tired and taking longer to recover from the heart decelerations the lack of blood flow caused. They called this 'late decelerations'. Basically he was in distress and not getting enough oxygen. The surgeon gently started talking me through the fact that the baby would not be able to emerge vaginally in the position that he was in and strongly recommended a c-section. Like her little hands, her demeanor was gentle, I think being respectful of the fact that I really wanted a natural birth. I panicked about how much time we were wasting talking through it and quickly and cut her off saying, 'Let's just keep him safe, let's do it.' She looked relieved. Someone threw some scrubs at V, told her to grab a camera and they started prepping me for the OR. Amusing side note - V is VERY modest normally, but actually walked out into the room in her underwear asking for different size scrubs because the trousers were too small. It was that kind of forget-yourself crazy. Also, during the crazy, I realized that I really needed to pee! I told someone who said I?d be given a catheter very soon ? I told them that if I couldn?t empty my bladder immediately I?d probably wet the bed. They told me that I couldn?t move off of the bed because I needed to stay connected to the monitors. Someone stuck a bucket under my bottom and I squatted, on the bed, with the door open with people coming and going throughout. They evidently forgot about me squatting on the bucket having contractions, and V?s mum was my hero. She loudly ordered someone to help me off of it. Somewhere along the way I heard someone say that I was dilated to 7cm. From arriving at the hospital to the incision was about 30 minutes. Our friend is a NICU nurse and said that in the medical field they call this a 'crash' c-section, and I can see why.
The OR was scary, but probably quite routine. I had a couple of contractions on the way and while the anesthetist was administering the epidural, which wasn't much fun, good news is that the pain subsided quickly after that. V was able to hold my hand the entire time, and was allowed to watch when he was born, then ran over to OR basinet with video camera in hand, and 4-5 NICU people were waiting to work on him. V was standing there asking if he was OK, but every person at that basinet was so busy working on him that nobody answered her, the baby was limp and gray. At this point V shut off her video camera. His initial apgar was 5 but he recovered really well for the second and was 9 ? for which I am so so grateful. V carried him over so I could kiss him on the forehead; all bundled up - so no immediate skin to skin time, which made me a little sad. He came out looking like he'd done 12 rounds in the boxing ring from where his face was being pushed against my cervix during contractions. His right eye was swollen completely shut. The baby was brought to me for skin to skin as soon as I hit the recovery room, about 30 minutes after he was born. I was so nauseous from the narcotic in the epidural that I couldn't look down at him for the first night. I did practice getting him to latch with the help of some nurses.
To end off (yes, finally!) Despite things not going according to plan, I am so incredibly grateful for modern medicine. We have our healthy and perfect little boy, I am recovering really well and we are bonding so well as a family. The hospital provided exceptional care to us, and V was able to room in with us for the entire stay. Breastfeeding is going very well, and he's gaining back weight a little bit ahead of schedule. Our midwife stayed with us and helped me through contractions right up until I was taken to the OR, the doula didn't make it in time for us.
Baby Alarico and I the day after he was born
 [/URL]
[/URL]
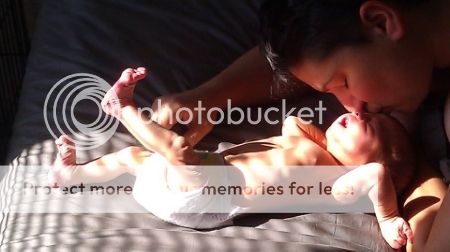
Alarico and V on our first morning home, just loving each other in a puddle of sunshine on our bed ![]()
 [/URL]
[/URL]
Alarico just being adorable
 [/URL]
[/URL]
Bonus picture! This boy is a milk hound, so this onesie totally applies ![]()






Re: Baby Alarico's Birth Story
Soo... cute! Congrats to you both
Married in September 2010, started TTC journey November 2012
Me-
7 IUI- 2 CP- 2 BFN
RPL blood work 12/27, showed a balance translocation in chromosome 11;22
Spouse-
PCOS 4 IUI-4 BFN
New Plan: Reciprocal IVF, me as carrier wife's eggs. Just went through insurance and received partial approval, so my part will go through my IVF benefits and wife's part will be out of pocket. Now just finalizing finance plans to cover the oop costs. Doctors office is in process of moving to a new building so there are no IVF start ups until March/April 2015.
Baby Oliver born 11/27/13
TTC stats with donor sperm...
IUI #1 with trigger, 1/4/13 - BFN
IUI #2 with trigger, 2/1/13 BFN
IUI #3 with tigger, 2/28/12 BFP EDD 11/21/13
We're queer. I'm 33, have severe stage 4 endo, and had both fallopian tubes removed. My love ("Manada" on the boards, 32) was diagnosed with diminished ovarian reserve. We did Partner IVF (my eggs, her uterus). We lost our twins Tavin and Casey at 21 weeks gestation.
Our IUIs
with @Manada: IUI# 1-7 (December 2012- September 2013) all BFN. Tried natural, femara, clomid, puregon/follistim, clomid and menopur combo, both the ovidrel and HCG triggers.
Our IVFs:
IVF #1 my eggs November/December 2013: Cancelled IVF due to poor response
IVF #2 my eggs/Manada's uterus January/February 2014
BCPs and lupron overlap Stimmed: 1/22-2/2: Bravelle and Menopur (dosage ranged from B300 and M150 to B375 and M150 to B300 and M225)
2/4 retrieved 10 eggs. Endo was much worse than expected. Only 3 eggs fertilized; February 7 transferred two day 3 embryos, froze one. All great condition.
BFP eve of 6dp3dt; Beta 1 (11dp3dt): 110; Beta 2 (13dp3dt): 175; Beta 3 (15dp3dt): 348; Beta 4 (19dp3dt): 2222; Beta 5 (21dp3dt): 4255
1st ultrasound (3/6 6w 1d): TWINS!!!! Twin A measuring 6w1d with a heartbeat of 118bpm. Twin B measuring 6w0d with a heartbeat of 113bpm.
***July 18, 2014 we lost our beautiful babies at 21 weeks gestation. They were born too early. Tavin Sara T. and Casey Elizabeth T. are beautiful and precious and we will love them and miss them forever.***
FET #1 December 2014
TTC with RE since March 2012
3 missed O's, 6 IUIs = 1 BFP then 8 w M/C, 5 BFNs
(2 unmedicated IUIs, 2 clomid IUI, 2 femara IUI)
Shared maternity/partner IVF, transfer #1 BFP!
EDD 11/28/13
Married to M and proud mothers to Olivia and Elise (8/19/2014) and to our fur-babies: Capone (pitbull), Jax and Atticus (cats)
Me - 30, My wife - 31 , Together for 10 yrs - Married August 2012
5 medicated IUIs w/ RE (March - July 2013) = BFN
Fresh IVF Cycle in September 2013 resulted in 18 mature eggs, 16 fertilized, 12 made it to day 5. Transfer of 2 Grade A blastocysts on 9/15/13, and 10 embryos in the freezer! *****BFP on 9/25/13 - betas: @10dp5dt = 232; @12dp5dt = 465; @15dp5dt = 1,581 *********William George born June 4, 2014*********Lbugher I will definitely still have a birth plan next time around. It tells your caregivers what your wishes are, even in the event of a csection.